Disclaimer: This article is for informational purposes only and is not medical advice. If you suspect an active COVID-19 infection or Long Haul COVID-19, please seek medical care from a licensed physician.
The Delta wave of the American pandemic has been with us for a while now. Nature and human folly have been hard at work rolling out this exciting new product line. Delta roiled India, the UK, and is spreading like wildfire across the United States. Designated a Variant of Concern by WHO, CDC, and many other agencies, Delta is known to be much more infectious and possibly more deadly than anything we've seen yet. Now, the unhappily exciting Omicron variant is having its worldwide release.[1]
Yet, it is not only hospitalization and death that should concern us. It is beginning to be acknowledged, but far from universally known, just how much damage coronavirus disease wrecks on the human body. Multiple organ systems are implicated: the nose, brain, heart, lungs, kidneys, ears, gastrointestinal tract, the pancreas, and reduced immune system function. Even mild cases of COVID-19 can cause lasting damage that doesn't reveal itself until later. These concerns should guide how we think about mitigation and elimination strategies.
It is unfortunate that we talk about this disease’s severity in terms of “assymptomatic”, “mild”, “hospitalized”, “ICU”, and “dead”. The majority of people will fall into the first two categories where the word “mild” perfectly obscures what may be quite large amounts of acute suffering and chronic symptoms. It also seems to send the message that “we don’t care about you because you aren’t dead”.
The literature is too complex to do more than introduce the impact of mild disease on one of these organ systems. Thus, in this article, I will review some of the evidence for brain injury in the hopes of demonstrating that this is a disease we cannot live with. In the articles I read, it seems to be accepted within the scientific community that damage is occurring, the main questions are exactly how much, by what mechanism, and whether it is reversible.
While I believe the government would like to end the pandemic, to the people in charge, this is more of a fantastical ideal than it is a serious project of elimination. With some justification, they are heavily relying on vaccines as a technological quick fix. However, instead of taking advantage of the opportunity the unexpectedly good vaccines gave us, they are attempting to reopen the economy even as caseloads rise, sometimes exponentially sharply. While blue states have been overeager to reopen, some red states have made them look good by comparison by for all practical purposes acting suicidally—not only reopening but banning or attempting to ban mitigation measures. In some states, Intensive Care Units (ICUs) filled up and the worst case occurred where hospitals were not able to service other ailments and people died that had nothing to do with COVID-19.
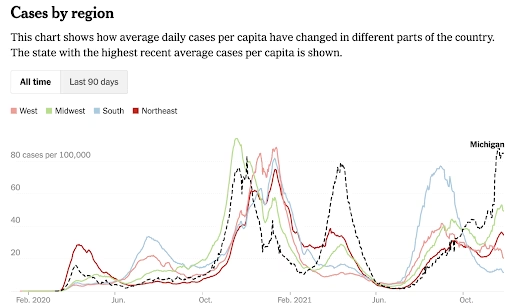
While the current wave appeared to be receding in the U.S. during much of the fall, my wary suspicion is that this is a combination of luck and an artifact of the transition from summer to winter. In the south, hot days cause people to stay indoors. In the north, cold days have that effect. Our national epidemic already shifted north and west, and now it shifts east. Most of the decline has come from the southern states. After its bountiful summer harvest, the reaper is settling in for a new season. Winter is coming.
Nonetheless, it is apparent that much of the public is exhausted of the pandemic and wants to move on; I've seen even organized socialists and professional scientists behaving as if the pandemic is almost over. As a reopened United States enters the winter months under the thrall of this virus and anti-scientific thinking, it's worth examining what we are really facing without flinching from under-appreciated and serious aspects of coronavirus disease.
In my reading, severe COVID-19 has been called “...probably amongst the most complex of medical conditions known to medical science.”[2] If we already knew everything we needed to know about this disease, it wouldn’t be the globe-altering problem that it is. We must have the humility to look earnestly and openly at what makes this virus and the syndrome it causes different from our prior experiences.
There are several aspects to SARS-CoV-2, the virus that causes COVID-19, that are under-appreciated in the public discourse. These relate to long-term disability and to the evolutionary potential of the virus (which we are now experiencing with the emergence of the Omicron variant). Both are worsened by uncontrolled proliferation of the virus, which is what a full reopening of the economy will accomplish.
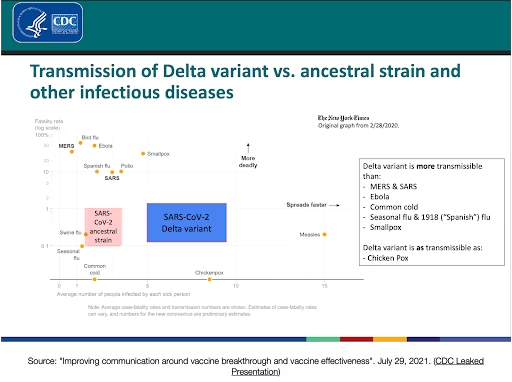
Nonetheless, such high viral loads mean they can transmit the virus, presumptively at similar rates to an unvaccinated person. If the vaccine prevents infection about half the time or less, but Delta is twice as infectious, have we gained anything on the transmission front since March 2020? With the emergence of Omicron, will we see progress on transmissibility go in reverse? The question then is, if hospitalization and death are to a large degree put at bay is it acceptable for everyone to catch COVID-19? In the absence of further information, one might be inclined to conclude yes and reopen the economy so we can get back to smiles, parties, and producing profits for the oligarchy (and organizing the working class in person).
However, in this piece, I aim to lay out a case for why this is not an acceptable course of action based on the Precautionary Principle. The principle has multiple formulations, but a popular one is found in the 1998 Wingspread Statement on the Precautionary Principle:
When an activity raises threats of harm to human health or the environment, precautionary measures should be taken even if some cause and effect relationships are not fully established scientifically. In this context the proponent of an activity, rather than the public, should bear the burden of proof.
Instead, I advocate that our primary global health strategy should be regional and eventually global elimination of COVID-19. We should also have two secondary mitigation goals: (a) minimize each individual's lifetime number of cases of COVID-19 (b) maximize the amount of time until first infection for as many people as possible. More on these later.
I hope to convince you of the less recognized dangers of the disease by presenting illustrative pieces from the scientific literature. To be clear, I am not an expert in the field. I have some scientific training at the undergraduate level and have been working in science for years, but I am not a Ph.D. nor do I work in this field. I have some background coursework in cell biology and genetics at the college level. Nonetheless, over the past four months, I've read about fifty papers on COVID-19 to try to get a handle on how these highly important but under-discussed topics might affect us once we get past the immediacy of ICU overflows.
I hope to communicate that within the scientific literature I reviewed, Long COVID, especially among mild cases, was naturally less frequently addressed than acute management in severe cases. However, it was taken seriously and was well known to impact multiple organ systems including the brain, lungs, kidneys, and heart. The precise mechanisms by which damage is done and the length of time that the damage will persist are still being debated, but substantial fractions of the population will encounter them. The mechanisms of damage are somewhat more obvious in severe cases than in mild cases.
Long COVID is also much more well studied in adults than in children. Therefore, while the disposition of schools is a burning issue right now, I will defer the objective treatment of this question for now, both because it would make this article too long and because the data are more difficult to interpret. I believe the Precautionary Principle nonetheless applies in full.
Without further ado, let's start peeking into the literature.
Incidence of Long Haul Covid
It is starting to be acknowledged that almost a quarter of infected individuals will suffer from Long Haul COVID, a constellation of symptoms affecting many different organ systems. According to a June 2021 study of 34 billion U.S. health care claims by Logue et al for FAIR Health,[3] 23.2% of all patients who had a diagnosis of COVID-19 subsequently developed one or more additional problems. This increased with severity. About one in five (19%) asymptomatic patients, more than one in four (27.5%) of symptomatic, and one in two (50%) hospitalized patients developed at least one new problem. This study excluded people with certain serious pre-existing conditions like cancer or HIV on the presumption it would skew the numbers worse. They found that there were at least fifteen post-COVID conditions affecting more than 1% of patients across all age groups. The top five were pain (~5.1%), breathing difficulties (~3.5%), hyperlipidemia (~3%), malaise and fatigue (~2.8%), and hypertension (~2.3%).
It's important to remember that while a COVID-19 diagnosis claim can be generated by suspicion-free testing, post-recovery problem claims are generated by a patient. This means they were experiencing enough difficulty that they sought medical help in a country where most people put off engaging with the American medical system as much as humanly possible. That means the reported pain, for the most part, considerably hurts and the breathing difficulties are fairly substantial. Hyperlipidemia (obesity) and hypertension could be assessed via a routine physical, but malaise and fatigue are self-reported. Most people try to sleep off a little fatigue – to seek medical help means it is persistent and bothering them. Regarding pain, it is difficult to know when it will resolve, but it certainly puts these people at risk of developing an opioid addiction if it is severe, becomes chronic and/or additional injuries intensify it over time to the point that such drugs are prescribed.
However, there are several other concerning categories that make the list in the top 15 (all have an incidence of over 1%): Anxiety (2%), Depression, Sleep Disorders, Intestinal Issues (2%), Skin Issues, Abnormal Heart Results, Abnormal Organ Tests, High Levels (Glucose, Cholesterol, Blood Pressure), Migraine/Headache, and GERD. These are all problems that either seriously interfere with your quality of life or reduce your expected lifespan. This study also found gendered differences in the frequency of certain problems (e.g. more heart disease for males, more thyroid issues for females). Patients that were symptomatic were 2.9x more likely than asymptomatic patients to die 30 days or later after first being diagnosed with COVID-19.
At this stage, it is too early to know how vaccines will affect Long Haul COVID-19, however, it seems reasonable to expect that most vaccinated people will do as bad or better than the asymptomatic or symptomatic groups. In "Covid-19 Breakthrough Infections in Vaccinated Health Care Workers", which appeared in the New England Journal of Medicine[4], the team found that during the surveillance period between January 20 and April 28 in 2021, 39 breakthrough infections (meaning RT-PCR positivity) occurred among 1497 fully Pfizer-BioNTech vaccinated Israeli health care workers (0.4%), 19% had persistent symptoms beyond 6 weeks. Five workers took a leave of absence longer than two weeks and one took leave longer than six weeks. 85% of the samples tested were the Alpha variant. While the study did not distinguish between asymptomatic and symptomatic breakthrough cases for this statistic, 19% does accord somewhat with the FAIR Health assessment for asymptomatic cases. The results of this study are concerning despite the low breakthrough rate because of documented waning in vaccine efficacy at preventing infection as the months tick by and the increased infectiousness of the Delta variant. A slightly newer study based on self-reports from the COVID Symptom Study app between Dec 8, 2020, and July 4, 2021 found a decrease in persistent symptoms after 28 days in breakthroughs of fully vaccinated people compared with unvaccinated people.[5]
Still, with large numbers of people unvaccinated, we don't even need to speculate. The population burden of having huge numbers of people with new potentially chronic health problems is a disaster that could linger for decades even if the virus is eventually eradicated.
Brain Involvement
The FAIR Health study showed that ~2.8% of patients diagnosed experience malaise or fatigue. It has been common to read news reports of recovered COVID-19 patients reporting low energy, "brain fog", difficulty concentrating, and trouble finding the right words (some to the point that they can no longer do their jobs as well). COVID-19 is seen by many as primarily a lung disease and perhaps secondarily as a disease of the blood vessels.
In this section, I aim to show that there is sufficient evidence to believe that COVID-19 can cause irreversible brain damage. While the scientific community is still coming to agreement on this, I believe the evidence accumulated so far is sufficient to presumptively hold this belief and act on it. There are multiple proposed non-mutually exclusive mechanisms for this brain damage including direct viral invasion of neurons, deprivation of olfactory sensory input, immune dysfunction, and lack of oxygen (hypoxia) due to respiratory or vascular damage. While our practical choices may be more restricted, the biophysical characteristics of the pandemic force us towards the poles of irreversible mass infection and highly mobilized active combat of the virus. Based on the Precautionary Principle, it is only necessary to prove that it is more likely than not true that COVID-19 causes irreversible brain damage and revise our position as the scientific record develops in order to commit ourselves to action.
I will meet this standard by first presenting a UK study wherein large scale online intelligence testing shows cognitive deficits in even mildly symptomatic COVID-19 patients and increases in the size of deficit in positive correlation with disease severity. Second, I'll demonstrate that an in-person study in Ecuador shows similar results. Next, I will show another study of the UK population, where brain imaging via Magnetic Resonance Imaging (MRI) showed reductions in gray matter for even mildly symptomatic patients. Fourth, I will show multiple studies that use PET scans to document slowed metabolism (hypometabolism) in the brains of adults. Lastly, I will show that there are multiple mechanisms that can account for that damage.
Cognitive Deficits
In July 2021, an article was published in EClinicalMedicine titled "Cognitive deficits in people who have recovered from COVID-19" by Hampshire et al.[6] This was a UK team that had just happened to be running a large scale online cognitive assessment on the British public that was widely advertised as "The Great British Intelligence Test" in cooperation with the television network BBC2 Horizon in order to help establish a baseline for cognitive function across many demographics. The data collection period covered December 2019 to December 2020. They highly promoted the assessment once in January 2020 and then again in May 2020. During the run-up to the second promotional push, they realized they could slot in a voluntary unadvertised COVID-19 questionnaire at the end of the test to see if COVID-19 affected cognitive function. They found that it did.
The experiment consisted of nine validated types of puzzles administered over the internet that were designed to measure spatial problem solving, spatial planning, working memory, spatial short-term memory capacity, visual attention, mental rotations, analogical reasoning, rare word definitions, and facial emotional discrimination. However, it was not a formal IQ test. 81,337 individuals completed the test and COVID-19 questionnaire with 93% indicating UK residence. 12,689 indicated suspected or confirmed COVID-19 spanning all severity levels, 386 people reported a positive biological test including 86% of self-reported hospitalized patients. The results were corrected for a variety of factors including age, sex, handedness, first language, education, country, occupation, and income.
The results were striking. For each qualitative increase in disease severity, a decrease in cognitive performance was found. Bio-confirmed COVID-19 showed more decline than mere suspicion. Importantly even the lowest severity cases measured, "Symptoms but without respiratory symptoms", showed declines. The finding for ventilated patients is less surprising as cognitive declines have been noted before as a general phenomenon. However, taking lack of oxygen to the brain as a possible reason doesn't adequately explain the non-respiratory symptoms case. Does this mean some patients had low oxygen saturation but didn't notice or misreported their category? Does it mean something else is at play?
Regardless, under our current set of circumstances, these self-reported results seem to suggest that even mild infections can cause declines in function—infections so mild that patients did not request even at-home medical assistance. Asymptomatic patients were not scored here, but symptomatic illness with and without respiratory symptoms is not uncommon with vaccination.
Online studies should be taken with a grain of salt because the experimenter never saw their subjects in person. Another study, "Cognitive decline among individuals with a history of mild symptomatic SARS-CoV-2 infection: A longitudinal prospective study nested to a population cohort " by Del Brutto et al from February 2021 adds some more confidence to this result with in-person clinical practice.[7] It was a longitudinal study conducted in the village of Atahualpa, Ecuador that had been following its subjects since 2013 with MRIs, EEGs, and cognitive assessments. When the pandemic hit, they started looking at 93 patients that had antibodies (“seroconverted”) and evaluated them using the Montreal Cognitive Assessment (MoCA). The MoCA is not a hard test, it consists of items like drawing a clock and naming animals (an example can be found here).
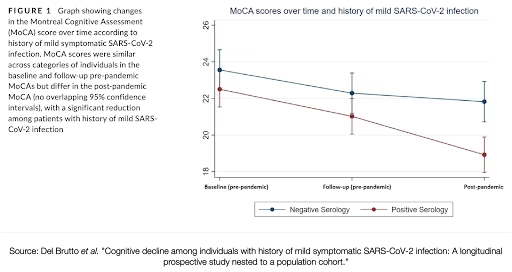
Based on the previous testing of the population, they knew that the average decline over the last nearly four years had been less than two points on this test. They considered a post-exposure decline of four points a symptom of cognitive impairment. The patients were older, 62.6 ± 11 years, leaned female, and a good proportion of them were diabetic, obese, had high blood pressure, had poor sleep, and some had depression.
Nonetheless, the 41 subject seronegative population and the 52 patient seropositive populations had similar MoCA scores pre-pandemic, but significantly different scores post-infection. 12 patients had declines of more than 4 points. This broke down as 11 out of 52 (21%) seropositive patients with a history of mild COVID-19 and 1 out of 41 (2%) of the seronegative subjects.
This study found no abnormal MRI imaging, but did find abnormal EEG. They found no detectable viral genetic material in the patient's cerebral spinal fluid, but they did find biomarkers for inflammation at 3 weeks after disease onset.
The authors noted that mild cases showed more than 18 times the odds of developing cognitive decline compared with their controls. The decline was subclinical, meaning the majority of patients and their close family members hadn’t noticed the cognitive deficit, but it could have long-term implications as they age.
While the study was unable to draw conclusions on what was causing the problem, they speculated that the declines could be due either to a delayed effect of the virus on the nervous system or to chronic immune dysregulation resulting from infection.
Gray Matter Reduction Found in UK Longitudinal MRI Pre-Print
In late June 2021, a pre-print (not yet peer reviewed) article appeared on medRxiv titled "Brain imaging before and after COVID-19 in UK Biobank" by an Oxford, NIMH, & Imperial College of London team.[8] UK Biobank had been routinely conducting brain scans using a variety of MRI-based technologies and had previously scanned the brains of over 40,000 human subjects before COVID-19 started. The patients were also assessed with a battery of basic cognitive assessments.
MRI techniques use very strong magnets to map the location of hydrogen, a plentiful component of water and fat, in the brain and create structural maps. A variant technique, Diffusion-Weighted MRI, uses pulses of magnetic energy that cause hydrogen to spin in alignment in areas where liquids are unable to move, enabling their detection; this can help identify areas of tissue damage by marking areas with increases in liquid diffusion where there shouldn’t be.
Starting in February 2021, they invited 785 subjects aged 51-81 years back for a second visit (an average of 38 months later) with 401 having tested positive for SARS-CoV-2. Only 15 of these had been hospitalized and of them only 11 with COVID-19 being the primary cause of hospitalization. That is to say, these were mostly "mild" cases. The diagnoses were primarily sourced from antigen tests linked from public health records and home lateral flow tests, so one weakness of this study is a lack of independent PCR confirmation. The date of diagnosis was spread through the time from the start of the pandemic in January 2020, but the majority were diagnosed after September 2020. Apart from hospitalization, the patients were not stratified by severity as scores on items like O2 saturation during their illness were not available.
On the cognitive battery, they found on a simple Trail Making Test (example) that the completion speed decreased in the infected group and the size of the decrease was larger for older patients. The gap was fairly small up to between ages 59-63 and then became fairly large reaching ~10-30% in the oldest. The results were significant even after excluding hospitalized patients. Oddly, of the six tasks in the assessment, it seems they only found a difference worth commenting on in one of the tests. It seems on the assessments measuring reaction time, fluid intelligence, or whether a puzzle was solved at all there wasn’t a difference.
In the MRI results, they identified “...atrophy and increased tissue damage in cortical areas directly connected to primary olfactory cortex, as well as to changes in global measures of brain and cerebrospinal fluid volume.” Some brain regions decreased in size, while others increased.
Thousands of brain regions were compared across the different groups. The region that survived the most conservative statistical test[9] in the non-hospitalized group was the temporal piriform cortex functional network, which is involved in processing the sense of smell. When a slightly more liberal statistical test was employed[10], other regions of the olfactory and piriform cortex showed significant changes as well as the parahippocampal gyrus (involved in processing visual scenes) and the left orbitofrontal cortex (involved in decision making). If hospitalized patients were added back into the comparison, five additional regions passed the more conservative test. The size of the changes between the patient and control groups were small, on the order of one to a few percent difference in thickness, with a greater difference with increasing age (though the relationship was not strictly linear).
Another discovery in the non-hospitalized patients was (under the more liberal test) an increase in Cerebrospinal Fluid (CSF) volume and a shrinkage of the superior frontal-occipital fasciculus (under the more conservative test). When hospitalized patients were added in, other results became significant such as a shrinking of the ratio of the brain to the intracranial space and an increase in the size of the right lateral ventricle (ventricles are fluid-filled spaces in the brain).
The brain region-specific results seem to indicate shrinkage primarily to the centers that process the senses of smell and taste. Diffusion-weighted imaging, a proxy for damage, indicated changes in these regions as well. The increase in CSF volume seems to imply diffuse damage across the brain. Exploratory visualization of differences in the diffusion-weighted imaging showed hotspots of apparent damage in multiple areas of the brain, including “Area G” of the insula, which is called gustatory cortex and is involved in processing taste. They found their measures of cognitive decline correlated with atrophy of crus II, a cognitive lobule of the cerebellum.
The authors speculated as to what could cause these issues. While they characterized direct viral invasion via the nasal mucosa as “heavily-debated”, two other possibilities seemed plausible. Many COVID-19 patients lose sensitivity to taste and smell during their illness, some losing it entirely. This loss of sensory input could cause the relevant brain regions to atrophy and has been documented in other research (if the sense of smell is recovered, some recovery in the brain regions may be possible). Another possibility would be virus-induced chronic neuroinflammation caused by the immune system.
In the discussion, the authors write of their concern that these results could foreshadow a future contribution to Alzheimer’s disease or other dementias:
The overlapping olfactory and memory-related functions of the regions shown to alter significantly over time in SARS-CoV-2, including the parahippocampal gyrus/perirhinal cortex, entorhinal cortex and hippocampus in particular, raise the possibility that longer-term consequences of SARS-CoV-2 infection might in time contribute to Alzheimer’s disease or other forms of dementia.
Indeed, they note that an international consortium is already being assembled to study the prospects of degenerative brain disease in COVID-19 patients.[11]
Long COVID Brain Region Hypometabolism in PET Studies
In 2020, in France, a team began investigating reports of brain complications in hospitalized COVID-19 patients using Positron Emission Tomography (PET) scans, a different technology than MRI. Using radioactive fluorodeoxyglucose sugar as a tracer, glucose sugar being the main fuel for brain activity, PET is able to directly watch the rate of sugar consumption to estimate brain activity. They looked at two severe patients initially (in comparison with more healthy controls)[12] and then followed up by looking at a more sophisticated retrospective study of 35 Long COVID patients and 44 healthy controls collected from before the pandemic.[13] These studies were between subjects instead of following the same people over time and the retrospective nature means certain biases, e.g. recruitment, cannot be excluded. The findings should be considered preliminary and exploratory.
Their experiment specifically looked at people without MRI or CT scan identifiable lesions on their brain; people that should have normal functioning brains. They instead found that while the tissue was grossly intact, there was obvious evidence of slow metabolism in several brain regions. In the discussion they state:
Our findings reinforce the hypothesis of SARS-CoV-2 neurotropism through the olfactory bulb and the possible extension of this impairment to other limbic/paralimbic structures as well as to the thalamus, the cerebellum, and the brainstem within these highly connected regions. The neurotropism of SARS-CoV-2 is first supported by cerebral complications already reported during the acute phase, such as strokes and encephalopathy/encephalitis. In the longer term, a delayed outbreak of psychiatric and neurological diseases of neuroinflammatory origin has also been anticipated. This neurotropism is overall concordant with previous findings reported for other coronavirus infections, with demonstration of the presence of the virus in the brain and in the cerebrospinal fluid. In this line, a recent meta-analysis reported psychiatric and neuropsychiatric presentations associated with severe CoV infection in more than 40% of patients in the early phase, and around 30% have post-traumatic stress disorder in the post-illness stage, with a chronic fatigue syndrome and fibromyalgia association.......patients with memory/cognitive impairment and more numerous complaints were younger. The relationship with age should be particularly noticed, especially because young people are supposed to develop a more benign form of the disease, which does not seem to be the case for these delayed/persistent functional complaints, even if we cannot exclude a bias of recruitment.
A third PET study, "Cognitive impairment and altered cerebral glucose metabolism in the subacute stage of COVID-19" by Hosp et al performed in Germany looked at 29 hospital patients that had a confirmed infection, loss of smell or taste, and new neurological symptoms (diagnosed in part based on MoCA scores).[14] They were examined soon after they were no longer infectious. In a group that was pre-selected for already showing cognitive symptoms 13 of 29 patients were MRI scanned and in 4 patients (30%) microembolic subacute infarcts were observed. 15 of 29 patients were PET scanned and 10 out of 15 (67%) showed pathological hypometabolism in some brain region. One patient died for other reasons and neuropathological examination revealed no neuroinflamation, but lots of white matter microglial (cells with scavenging and immune functions) activation.
The authors noted that there their images did not seem to be consistent with active encephalitis. Combined with pathology which showed innate (non-specific) immune activation, dysregulated immune signaling (cytokine) could lead to the cognitive impairment and hypometabolism witnessed. This is similar to what happens in septic bacterial infections, which cause problems clearing cellular debris and circulatory problems.
While the picture will continue to become clearer, it seems that some COVID-19 patients do have some amount of brain impairment. The scientists in these two studies seem to favor different hypotheses about what might be causing it: neuroinvasion by the virus in the former and immune dysregulation in the latter, though neuroinvasion is considered seriously later in the text.
These studies aren't conclusive, but they are nonetheless concerning, especially in light of the documented losses of cognitive function. It is hard to say whether these results foreshadow what may be an increased burden of Alzheimers, dementia, and other neuropsychiatric problems in the decades ahead. If the problem is mostly confined to a prolonged immune response without lasting damage, perhaps the syndrome will be reversible.
Proposed Mechanisms of Action in COVID-19 Cognitive Deficits
The FAIR study of medical claims showed that complaints of long COVID are highly prevalent among anyone that had a documented COVID-19 diagnosis, with increasing complaints accompanying increasing severity of disease. I have shown substantive evidence of functional declines in cognitive performance and physical evidence of declines in gray matter and slowing of brain activity in certain regions from MRI and PET imaging in patients with mild symptoms.
The last piece of the puzzle is to show one or more mechanisms by which that damage occurs. In the literature I reviewed, there seems to be consensus that COVID-19 patients do exhibit neurological involvement, but there isn't consensus on what causes it yet. In this section, I aim to show that there are multiple highly plausible mechanisms by which this damage can be caused and that it is more likely than not that one or more of these proposed mechanisms are in operation.
Before we get to that though, we need a quick tutorial on what is known about how SARS-CoV-2 infects cells and causes damage.
How does SARS-CoV-2 infect cells?
SARS-CoV-2 is a virus 60 nm to 140 nm in diameter[15] (compared with about 5µm to 150µm for a typical non-neuronal human cell) that is enveloped with a fatty membrane and is surrounded with Spike (S) protein. It latches onto an extracellular receptor Angiotensin Converting Enzyme 2 (ACE2) using its spike protein. ACE2 is important in the regulation of blood pressure and fluid and salt balance (the renin-aldosterone-angiotensin system). A virion latched onto ACE2 is then assisted by TMPRSS2, a human protein typically also present on the same cell, which cuts the spike protein to activate it.[16] The activated spike protein then inserts into the cell membrane and fuses the viral membrane to the host cell in a zipper-like motion. This process takes about 10 minutes in SARS-CoV-1[17]; SARS-CoV-2 uses a different faster entry mechanism.
The virus may also be able to use a more typical but much slower pathway using cathepsins[18] to enter the cell, mainly if TMPRESS2 is unavailable. There is also some evidence that SARS-CoV-2 may also be able to use an alternative pathway involving another cell surface protein CD147 (also known as EMMPRIN)[19]. The widely distributed cell membrane protein Neuropilin-1 (NRP1) may also enhance ACE2 interaction or provide an alternative viral entryway by interacting with furin cleaved spike protein.[20]
ACE2 is unfortunately located in a large number of different cell types all over the body in many organ systems notably including the nose, lungs, gut, heart, and some cells of the immune system. Until recently, it was thought that ACE2 was not expressed in significant quantities by brain cells. However, it was later found that while brain mRNA expression for (the assembly instructions for making) ACE2 is very low, ACE2 is expressed in protein form (the functional form) in greater amounts, more often in the cytosol of cells.[21] While less is known about NRP1’s relationship to the virus, it is also expressed in olfactory neurons.
Once inside the cell, the viral proteins and RNA hijack the cell's machinery and use it to produce about 100,000 new virions[22] over about 10 hours[17] which then travel to and infect neighboring cells. During the incubation period, the virus suppresses most ordinary protein production and hijacks the remainder. It forces the production of large quantities of viral protein Non-Structural Protein 1 (NSP1), which blocks the transmission of warning signals such as anti-viral interferon mRNA transcripts from the nucleus. On their way out, spike proteins are cut at the furin cleavage site, which prepares them to interact with TMPRSS2. More infectious variants appear to have a higher percentage of spike protein activated.
Sometimes infected cells expressing spike protein on their surface will fuse with and infect neighboring ACE2 carrying cells, creating multinucleate agglomerations called syncytia, a feature seen in the lungs of severe COVID-19 patients.[23] This is highly abnormal as most types of cells in the human body have only a single nucleus, with red blood cells (no nucleus) and muscle cells (naturally multinucleated) being major exceptions. Growing syncytia can capture nearby macrophage innate immune cells expressing ACE2[24] to further delay alerting the immune system.[25][26]
What is the Known Pathology of COVID-19?
How does SARS-CoV-2 cause disease? The pathology of COVID-19 is startlingly complex. Indeed, the comprehensive review by Marik et al noted that "...severe COVID-19 is probably amongst the most complex of medical conditions known to medical science."[27]
It is difficult to describe this condition accurately and comprehensively in a short space, so I'll describe only a few important elements and otherwise refer you to Marik et al's paper and the other references.[28]
SARS-CoV-2 usually enters the body via inhaled droplets or aerosols and attaches to the ACE2-rich epithelium in the upper respiratory tract, usually in the nose. There it incubates, about twelve hours later virions migrate to the lower respiratory tract and infect ACE2 positive epithelial cells in the alveoli of the lungs, the sites of gas exchange (mainly oxygen and carbon dioxide) between the atmosphere and deoxygenated blood. Patients who develop symptoms will usually also develop pneumonitis (inflammation of lung tissue), often bilaterally, which develops into Organizing Pneumonia which Marik et al describe as being distinct from Acute Respiratory Distress Syndrome (ARDS).
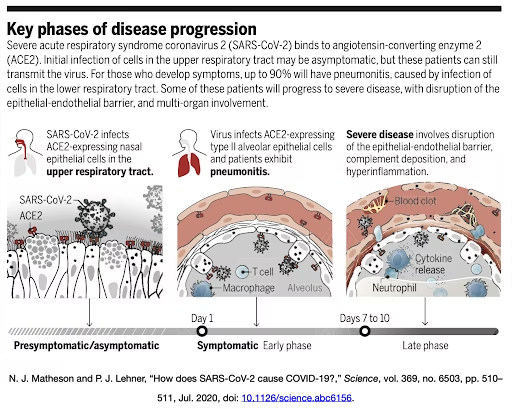
Severe COVID-19 is primarily a hyperinflammatory disorder of the immune system, in most patients the virus is long dead by the time they decline precipitously (see figures). The virus is able to replicate very quickly and suppress warning signals from cells, this enables very high viral load and a disorganized delayed immune response.
If the patient progresses to severe disease, usually occurring 7-10 days after onset of symptoms (suggestive of adaptive immune involvement), a breakdown of the barrier between the blood and the alveoli, fluid filling the alveoli preventing gas exchange, blood clots, complement deposition, infiltration of innate immune cells, and lung fibrosis may occur.[29] A systemic pro-inflammatory feedback loop promotes thrombotic formation that can cause infarcts in many organ systems.
The inflammation caused by the immune system degrades the lungs further and further, causing them to become fragile and reduces their ability to transport oxygen and carbon dioxide. The ultimate cause of death can come from the failure of many organ systems, but respiratory failure and heart failure are frequent.
Marik et al commented on the factors that might lead a person to develop a more severe disease course:
It is likely that the balance between viral inoculum size, rate of viral replication, the host production of interferons, and pro-inflammatory mediators determines the outcome of infection with SARS-CoV-2. Those patients who develop a brisk interferon response with an effective innate immune response likely rapidly eliminate the virus. However, rapid viral replication leading to high viral concentrations in the upper airways occur in those who are infected with a large viral inoculum and those who have a poor or delayed interferon response. The delta variant replicates to achieve very high concentrations in the nasopharynx and this likely accounts for its increased transmissibility and virulence.
Some of the factors in developing worse COVID-19 appear to be the size of the initial viral inoculum (number of viral particles) and the speed of the immune response. Therefore, it seems methods that reduce the size of the initial innoculum would be helpful (such as masks, especially high-quality N95 masks) and methods of accelerating the response time of the immune system (via vaccination) or delaying viral replication (via drugs). Conversely, this logic seems to imply that things that increase the size of the innoculum (e.g. not wearing a mask, poor ventilation) or accelerate viral replication (such as new variants) could be worse. While there is no solid evidence of this, there are a number of papers speculating to this effect and note that there does seem to be a strong negative correlation between universal masking and disease severity.[30][31][32]
The Proposed Mechanisms
How could SARS-CoV-2 cause the cognitive deficits and imaging oddities described above? In the literature, there seem to be five major proposals with various amounts of interplay between the elements: lack of oxygen in organ tissues (hypoxia), direct infection of the central nervous system (neuroinvasion), clotting, loss of sensory input, and immune dysregulation.
For severe patients, the ones that make it out of the hospital are not problem-free. An editorial by Baker, Safavynia, and Evered called "The ‘third wave’: impending cognitive and functional decline in COVID-19 survivors"[33] described the factors that would cause a hospitalized patient to face continued functional and cognitive decline. The number of factors all pointing in the same direction are depressingly large. This is very illustrative, but we're concerned with mild disease.
Hypoxia is known to cause cognitive deficits if patients stay in a deprived state for too long. In the hospital, this can happen both from the natural course of the disease where the lungs become too damaged to properly exchange gas even with high flow oxygen or from otherwise prolonged low oxygen saturation. However, this explanation doesn't make as much sense in mild cases where blood oxygen saturation doesn't fall dangerously.
Much effort has been expended looking into whether the virus is neurotrophic (able to infect neurons, the brain cells involved in nervous system control), and the answer seems to be yes, but only playing a minor factor in the evolution of severe disease. Early on, it was thought that neurons didn't express ACE2, which is necessary for infection, but it was later discovered that some neurons do.[34] Experiments by Song et al showed that viral replication was possible in human brain organoids (small brain-like structures grown from stem cells[35] in a petri dish) and small amounts of virus have been found in the central nervous system of patients post-mortem.[36]
Song et al also challenged mice with SARS-CoV-2 through their nose and found it was a clear infection pathway into their brain. Similar experiments with SARS-CoV-1 (the original SARS virus from 2003) found an infectious pathway to the brain via the nose in mice.[37] Another experiment looked into the cause of anosmia (loss of smell) and found that olfactory sensory neurons did not express ACE2 but the mechanically and physiologically supporting cells of the olfactory epithelium and respiratory epithelium did. This lead them to propose that damage to the epithelium could cause impaired functioning and death of the sensory neurons.[38]
So far neuroinvasion via the olfactory tract seems suggestive via several different lines of evidence, including the studies we discussed above, but far from conclusive and some lines of evidence are against it. Nonetheless, given the autopsy findings of viral infection in the brain, several other pathways have been proposed, sometimes based on the behavior of similar viruses or specific evidence for this virus. These include disruption of the blood-brain barrier allowing infected cells or fluid to access the brain and retrograde transport of virions from other areas of the body such as the gut[39] via the vagus nerve.
A review by McQuaid et al expressed that there is limited evidence for each neuroinvasion mechanism as a pathway for major neuroinvasion, but allowed that some amount could contribute to long-term consequences.[19] They wrote:
There are many possible ways the virus can affect the brain. The main way is due to dyspnea and thromboembolism that deprive the brain of oxygen and blood, and can lead to cerebral edema. Depending on the viral load, it can enter brain via retrograde transport along nerve endings in the buccal and nasal cavities, the main route of entry of the virus into the body. While the levels of SARS- CoV-2 in blood is low, from blood the virus can enter the brain via the normal or dysfunctional vasculature and access cells within brain, which express receptors that can interact with this virus. Interaction with ACE2 and/ or CD147 on cells of the NVU [Neurovascular Unit] could activate MMP9 that would break down the basement membrane, and render pericytes dysfunctional. The SP [Spike Protein] can slowly cross the cerebrovasculature via absorptive transcytosis, but not by ACE2. Entry into the CSF via the choroid plexus could distribute the virus to brain along the CSF drainage route. Virus could also enter brain with the trafficking of leukocytes. Thus, the aging brain may be a neurovascular target of SARS-CoV-2 with potentially devastating consequences, but there is no sound evidence of major neuroinvasion. In addition, the significance of neuroinvasion to the disease outcome in unclear since there is over- whelming respiratory failure in patients from which brain samples were tested for SARS-CoV-2. A long-term effect of this viral infection may be neurodegeneration and behavioral changes.
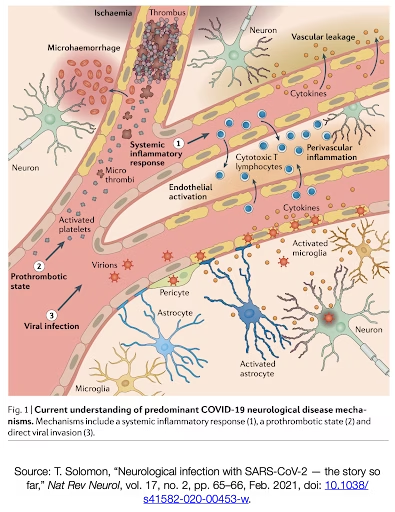
"Neurological infection with SARS-CoV-2 — the story so far" by Tom Solomon gives the clearest discussion I've found as to what might be going on.[40] Solomon points out three different pathways for causing neurological disease: (1) Systemic inflammatory response which leaks cytokines and Cytotoxic T cells into the brain (2) Prothromobtic state which causes clots and micro-hemorrhages to form (3) Viral infection which infects the vascular tissue and some neurons causing inflammation and activated microglia and astrocytes. He wrote:
In summary, if the retina is the window on the brain, then for understanding SARS- CoV-2, the nose has perhaps been the front door. For just as SARS-CoV-2 causes disturbance of smell without infecting olfactory neurons, evidence suggests that disturbance of higher mental function occurs predominantly without infection of CNS neurons. Although the virus can enter the brain, it seems to predominantly infect vascular and immune cells. Local inflammation up regulates astrocytes and microglia, perhaps compounding the effects of circulating pro-inflammatory cytokines in severe systemic disease. Microvascular infarcts and haemorrhages, which are part of the systemic coagulopathy and vasculopathy of COVID-19, are probably also critical in the development of encephalopathy, delirium and other neurological manifestations of SARS-CoV-2 infection.
As the majority of the effects described are due to some kind of vascular inflammation and immune response, we have to ask, does this occur in mild cases of COVID-19? As mild cases typically are not available for autopsy for obvious reasons, it's more challenging to answer this question. However, it is known that a majority of asymptomatic cases show evidence of Ground Glass Opacities on a Lung CT scan, which indicate areas of inflammation and pneumonia in the lungs.[41] It seems plausible that symptomatic cases would have even stronger inflammation, but direct evidence on brain vasculature may be lacking on this point.
Applying the Precautionary Principle
Now we must ask ourselves whether the Precautionary Principle is to be invoked. Does the balance of the evidence favor that there may be a persistent threat to human health caused by mild COVID-19 even if the scientific evidence is not fully conclusive? If hospitalization and death are to a large degree put at bay is it acceptable for everyone to catch COVID-19?
After this brief tour through the rapidly evolving literature, I hope to have convinced you that the balance of the evidence favors coronavirus disease being a persistent threat to human health. We looked at the incidence of Long Haul COVID, we showed that cognitive tests exhibited decline with both internet assessed and clinic assessed testing. We then showed that MRI, at least in the more powerful pre-print study, exhibited structural changes to the brain. Then, PET studies showed hypometabolism in the brains of COVID-19 patients with mild and hospitalized disease. Lastly, we reviewed the mechanisms by which the damage could be accomplished. Here, lay many different routes of infection and mechanisms of damage that are still being studied. Some of the proposed mechanisms are relatively irreversible (ischemic clotting), while others may be reversible (interference caused by prolonged glial activation).
This is exactly the situation the Precautionary Principle is designed to cover: evidence of hazard without a precise understanding. Therefore, it is logical to conclude it is not acceptable to infect the whole population. It is poignant to note that another article along these lines could have been written on the lung and cardiac implications of contracting mild COVID-19.
Can We Vaccinate Our Way Out?
Given it is not acceptable to infect the whole population, we have to find ways to minimize the impact of COVID-19. It is depressing to think about how it has gotten to this point when the pandemic could have been curtailed by strong action at the start, but nonetheless there are ways forward.
While the disease is resident in animal populations such as white-tailed deer and therefore difficult to eradicate completely, it should be possible to mostly eliminate it from human populations and clamp down on it when it pops up again. This has been somewhat successfully done in some countries such as New Zealand and Vietnam, though Delta has reduced the efficacy of this strategy with recent waves spreading there.
It's not possible to eliminate COVID-19 across an entire large region at once, so what might be realistic is to seed and grow sanitary zones until they are very large so that within them, we can switch back from mitigation (e.g. lockdowns) to containment strategies (e.g. test, trace, and quarantine all cases in the zone). In all cases, we need to get as many people as possible vaccinated.
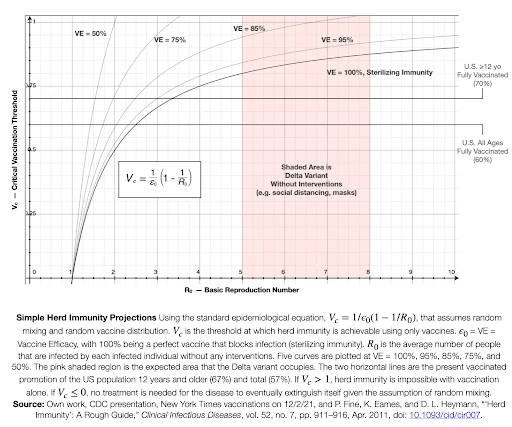
To give an idea of the magnitude of this task, there is an epidemiological equation that describes the number of people needed to be vaccinated in order to bring the pandemic under control.[42]
Vc is the critical population percentage to vaccinate to make herd immunity attainable, 𝜖0 is the vaccine efficacy, and R0 is the average number of people that are infected by each infected individual without any interventions. It assumes random mixing of the population, random vaccine distribution, and no other interventions. These are not realistic assumptions, but this artificial scenario provides a baseline for further reasoning.
The chart above plots five different scenarios where the vaccine efficacy (VE) is 100%, 95%, 85%, 75%, and 50% along with Delta's characteristics and the vaccination status of the US today. Post-infection immunity gives some protection, but it is not as well characterized. In May 2021, the CDC estimated that 120M people in the US have been infected (~36%). Some of them have gotten the vaccine too. There's some evidence that a substantial fraction of COVID-19 infections do not result in usable antibodies.[43]
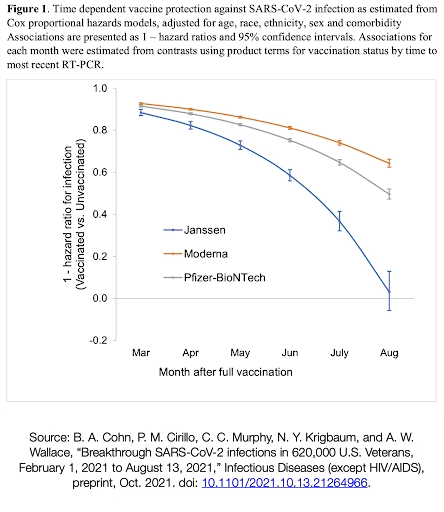
A recent pre-print study of 620,000 Veterans through the U.S. Department of Veteran Affairs health system tracked the efficacy of the three approved US vaccines (Pfizer-BioNTech, Modern, and Johnson & Johnson) over the period of March 2021 to August 2021 and found a substantial waning response in its ability to completely prevent infection (though they still were protective against hospitalization and disease).[44] The population in this study was older, so perhaps they were more vulnerable to this effect. Nonetheless, given that similar information has been coming out of Israel, this tells us that we can't necessarily count on high vaccine efficacy.
Boosters can rescue the level of protection, but it is not yet clear for how long they will last. However, there is a reason to think the boosters will be more durable than the first set of shots. Due to the emergency nature of COVID-19, the first set of shots was given on an abbreviated schedule that was likely still within the ambit of the primary immune response which lasts for weeks. Giving the booster months later, will guarantee that it will trigger a true secondary immune response which is more powerful. However, antibodies nearly always decline over time. If they didn't, your blood would turn to sludge from all the antibodies from different infections you acquire throughout your lifetime.
Looking back at the chart of simple herd immunity projections, we can see Delta is quite fierce. If we have a perfect vaccine, we would only need to get about 80-87% vaccinated to end the pandemic. However, if we have less than perfect vaccines, it is substantially harder. When the vaccines are at peak efficacy, they fall somewhere between the 95% or 85% VE lines where about 85-92% and 88-100% of the population would need to be vaccinated respectively to end the pandemic. For the 85% VE curve, if the transmissibility of Delta above about 6.75 additional people infected per a single infection it is impossible to end the pandemic through vaccines alone. As we can see from the veterans study, on average we may be at lower efficacy than those more optimistic curves. Below about 80% VE, it is not possible to end the pandemic through vaccines alone assuming the lower bound transmissibility of 5 additional infections per case.
This seems to pretty clearly indicate that to end the pandemic, we need to shift the effective transmission rate (move the pink shaded area left) in order to allow the vaccines to work their magic. A combination of universal vaccination and Non-Pharmaceutical Interventions (NPIs) like social distancing, air filtration, masking using high quality masks (e.g. N95s), reduced gathering sizes, work from home when available, and lockdowns in some instances. This will be a slog of establishing and maintaining sanitary regions with aggressive measures as seen in China.
When confronted with this, it seems clear why our bourgeois government officials have thrown in the towel and have decided we need to live with the virus – they aren't capable of withstanding the loss of profits and growth necessary to sustain human health. Nor are they capable of the mass politics and shift in institutions it would take to actively encourage the working class to combat this disease over the long haul. They also do not believe they can rely on other government and business entities to cooperate on a long enough time frame.
As more people become infected, they acquire more chronic illnesses and breed new variants of concern. This has been absolutely confirmed by the emergence of the Delta and now Omicron variants. Western governments created this situation in the first place by reacting with insufficient speed and intelligence at the beginning of the pandemic. Now, they continue to make it worse. Nonetheless, through active combat, we can still defeat Delta. However, if Delta mutates into an even more transmissible variant, it may push the shaded area so far to the right that our interventions won't push it far enough back and the virus will have effectively won and become endemic unless we can increase the effectiveness of other mitigations (such as by universal wearing of N95 masks).
There is little reason to believe that SARS-CoV-2 will moderate itself into a "cold" on any reasonably short timescale any more than we'd expect that of the highly mutagenic HIV/AIDS virus. However, universal vaccination will help prevent the horrific death tolls we have seen play out at the beginning of the pandemic, though the effects of mild COVID-19 that we discussed in this article may remain relevant.
Nonetheless, more optimistically, if we were to implement strong measures right now, if we can push Rt (the effective transmission rate) down to about 2.5 through NPIs, we could end the U.S. pandemic right now in many regions through the strength of our vaccination program. This may be within reach on a theoretical level as a meta-study of the effectiveness of NPIs found that reductions in the transmission of half to three-quarters were achievable by using all three of social distancing, mandatory masking, and quarantining infected patients.[45]
However, implementing these measures effectively may be difficult in the United States as anti-vaccine, anti-lockdown, and anti-masking sentiments are relatively high. A more likely trajectory would see creeping increases in vaccination status, with a jump after young children are approved, making a final push for elimination more practical in the higher vaccinated regions. Eventually, a final national push for elimination could be contemplated if vaccine waning can be effectively controlled through boosters.
Maintaining a national containment zone and eventually, worldwide elimination, will require international cooperation to defeat COVID-19s and the free distribution of the latest vaccine technology globally. A national border strategy is a natural fit to the contours of the political structures that are actually existing, but in the U.S. this would also be an excuse to exclude and torture South and Central American migrants (victims of U.S. terror campaigns in their native countries). We need to show solidarity to immigrants and make sure they are vaccinated both for theirs and our sakes, but in a country with a centuries-long history of abuse like ours, creative ideas are necessary to avoid invoking the misanthropic tendencies of our polity, most recently embodied by the Customs and Border Patrol (CBP) and Immigrations and Customs Enforcement (ICE).
Ideally, we could welcome immigrants at the border and offer them vaccinations at the port of entry, in part to compensate them for the U.S. inflicted economic damage and coups that drove them to migrate. However, this is unworkable as those borders are patrolled by deadly nativist terror squads. One alternative could be for each city to offer hotel quarantine services and free vaccination to all travelers regardless of visa or citizenship status. This would not only benefit Americans traveling between cities, but could act as a natural attractor for newly arrived undocumented people if ICE, CBP, and other federal police could be prevented from accessing those locations. Offering free vaccinations a short distance away from the southern border in partnership with Mexico could be another strategy. These are only off-the-cuff ideas, not hard proposals, and are offered only to jump-start a conversation.
Regardless of how things play out with herd immunity, there are two additional mitigation goals we should consider: (a) minimize each individual's lifetime number of cases of COVID-19 (b) maximize the amount of time until first infection for as many people as possible.
The reasoning for (a) is simple. Given that SARS-CoV-2 virus is already capable of reinfection in a small fraction of cases, and Omicron appears to have already demonstrated a high degree of escape, it seems likely that it may be able to introduce similar long haul damage as mild infection. If damage can accumulate over multiple infections, then it makes sense to think about minimizing each individuals' lifetime cases. For an individual, this means taking precautions to avoid becoming infected for as long as possible. On a policy level, one possible proposal might be to provide a means for workers to retire from high-risk jobs after they incur a certain number of infections.
Regarding (b), as the pandemic drags on, the public's exhaustion may lead some people to wonder why they are making sacrifices if they feel infection is inevitable. Why not get it over with? The history and nature of the pandemic clearly show why waiting is better. Firstly, avoiding infection reduces the transmission rate and helps achieve herd immunity. Secondly, in January 2020, there were no vaccines, no Remdesivir, no IV antibodies, no established medical practice for treating the disease, and insufficient ventilators. By November 2020, some IV antibody medications became available under Emergency Use Authorization (EUA)[46] and medical practice had improved outcomes somewhat. In January 2021, the first generation of mRNA vaccines became available in the US[47] and over the next year became widely available under EUA, though the variants of concern also revealed themselves. In August 2021, the first full FDA vaccine approval came through.[48] In November 2021, Molnupravir, the first (potentially real) oral drug treatment is being discussed for EUA at FDA[49] and is having doses being procured pending that authorization[50] (though there are concerns about its mechanism of action potentially causing increased mutation in humans and the virus). A second oral drug, PAXLOVID (ritonavir), with a different mechanism of action, was announced with plans to submit it for EUA.[51]
While the virus changes, our technology, and practices are changing as well. Could a more effective second generation of vaccines, the wide introduction of air filtration, or prophylactic pills eventually appear? Good things come to those who wait.
Conclusion
My belief is that surrendering to the virus is not an acceptable course of action. The clock is ticking and we must use our remaining window in order to defeat it. To do so would benefit all of us on both an individual and societal level. In a future article, I hope to cover the evolutionary potential of SARS-CoV-2.
It is unfortunate that the political structure of the United States is completely unable to cope with the demands of the pandemic. Capitalism and its imperatives are the main drivers of U.S. policy, an alien machine that ignores human needs that has evolved to become ludicrously short term in its planning. Sheldon Wolin wrote[52] that our political economy is one of inverted totalitarianism — dedicated to the demobilization of the working class in order to allow maximally undisturbed capitalist and imperialist action. While I don't agree with his aspersions on the nature of communism, he nonetheless made a useful comparison that helps illustrate the American system.
Communism, the traditional ideology of the streets, sought to mobilize the working class towards decent ends. Fascism was an innovation that found a way to create a highly mobilized popular base for horrific right-wing ideas, which traditionally had held sway only among the upper classes. The American system instead has found that it can retain stability by atomizing the public, demobilizing left-wing political factions, turning politics into spectacle, and plugging in the real choices from above through opaque maneuvering – totalitarianism, but without popular mobilization.
In a public health crisis of this magnitude, we must mobilize the public to combat the virus. Yet our system is incapable of doing anything other than what it has learned to do for decades: juice the economy using financial instruments and coercive tactics to get workers working (and discard them when unprofitable), even when they are counterproductive. This political structure stands in the way of effective action that would promote human health and flourishing. It has resulted in one of the world's worst outbreaks of COVID-19, even among the self-described capitalist world, in what is allegedly an advanced country.
As internationalists, we must recognize that what happens inside the U.S. and what happens outside of it are intrinsically linked. The pandemic has gone global so quickly and overwhelmingly due to the nearly completely globalized economy. Ships, cars, trains, and planes move people and goods, but also the disease, around the world at speeds and throughputs that have never before been witnessed in human history. Capitalism built this global trade system for several reasons: to expand global markets for goods and services, to exploit the cheapest global price of labor and extract the natural resources of far-flung deposits, to reduce the risk of strikes in the imperial core by moving essential manufacturing jobs to countries with weaker labor power, and to promote the US dollar as a global reserve currency by sending enough paper overseas for it to be useful in the global financial system while simultaneously acquiring material goods in exchange.
Socialists have always called for internationalism with the understanding that the asymmetrical power of capital to choose where to operate can only be balanced by cooperation among labor at each stage of the logistics pipeline from the extraction point of natural resources to their sites of manufacture, sale, and eventual disposal. Now that a deadly epidemic virus is transmitted bidirectionally along world trade routes, we need to recognize that control measures must be taken at both ends of the route. In a globally connected world, any instance of COVID-19 will eventually be transmitted back home and from home to every inhabited point on the globe. After all, the virus got its start in China, literally the other side of the world, and within months found its way here.
Therefore, it is absolutely essential that vaccine and other prophylactic technology be shared as widely and freely as possible, not only as shipments of doses, but the knowhow, materials, and personnel to manufacture them wherever it is advantageous. The U.S., as a vaccine-rich nation[53] that developed highly effective vaccines largely with public funds, must be pressured by socialists here and abroad to waive patent protections on the mRNA vaccines and compel the pharmaceutical companies to make their technology, doses, and staff available to every country on Earth as fast as possible. The international distribution system, currently implemented by the voluntary COVAX organization and individual bilateral agreements, should be replaced by a rationalized mandatory framework that prioritizes production and distribution based on need.
In concrete terms, this means as a first step pushing the U.S. government to go beyond supporting the TRIPS Waiver. We need to get them to pressure the pharmaceutical companies domestically to stop them from lobbying in the other countries holding vetos. I suspect the only reason the U.S. government supported the TRIPS Waiver is that they knew other countries would veto it. Don't let them get away with this trick. I doubt other NATO countries would oppose the U.S. in this if our government was serious. It would be a fruitful strategy to coordinate with socialists in the countries that hold the remaining vetoes.
While the socialist left in the United States has undertaken many admirable actions in response to the pandemic, mutual aid, prisoner liberation, and anti-eviction action prominently come to mind; I have been surprised that there has been comparatively little organized discussion of the pandemic as a political line or slogan. The capitalist governments are coping poorly with this world-historic challenge; we should be waving the bloody shirt. After all, the US government alone has allowed more than 719,000 people to perish in the official count as of October 15, 2021 (estimates of excess deaths that account for changes in behavior such as less driving are even higher, between 724,000 and 1,063,000) when many other countries, and all self-described socialist or communist countries (see table), managed to do multiples better. As of this writing, the U.S. is in 206th place out of 221 geographic regions in COVID-19 deaths per million people on the worldometers.info list.
The social choice our leaders have made is world-historically criminal. It would be to both the benefit of society and the struggle for socialism to continually point this out and convincingly describe the path to a world free of COVID-19 and the capitalist system that led us here.
Acknowledgements
This was a long piece to write taking four months of effort. Thank you to the editors of Cosmonaut Magazine for entertaining my multiple drafts and abnormal timelines for writing. I'd also like to thank Dr. Eric Feigl-Ding and the World Socialist Web Site, neither of whom I have a personal connection with, but surfaced the articles that initially piqued my interest in this topic. Thanks to Sudip Bhattacharya for his comments which improved the draft substantially. Special thanks to my girlfriend who put up with my late nights researching and writing while she performed ICU rotations, sometimes caring for COVID-19 patients, and probably could have used more of a break from work-type discussions.
William Silversmith is a member of the Central Jersey chapter of the Democratic Socialists of America and a longtime scientific software developer. You can follow him on Medium @willsilversmith or email him at first.last@gmail.com
Liked it? Take a second to support Cosmonaut on Patreon! At Cosmonaut Magazine we strive to create a culture of open debate and discussion. Please write to us at submissions@cosmonautmag.com if you have any criticism or commentary you would like to have published in our letters section.
- As I was finishing this piece, the Omicron variant emerged and appeared to exhibit very high transmissibility with concerns of escape from prior immunity. We’re in for another roller coaster ride folks. It’s too early to securely know the properties of this variant right now, so if it turns out to be a world-historic turning point in the pandemic, please mentally adjust the text as you read with your knowledge from the future. ↩
- P. E. Marik, J. Iglesias, J. Varon, and P. Kory, “A scoping review of the pathophysiology of COVID-19,” Int J Immunopathol Pharmacol, vol. 35, p. 205873842110480, Jan. 2021, doi: 10.1177/20587384211048026. ↩
- Logue, J. K. et al. Sequelae in Adults at 6 Months After COVID-19 Infection. JAMA Netw Open 4, e210830 (2021). ↩
- Bergwerk, M. et al. Covid-19 Breakthrough Infections in Vaccinated Health Care Workers. N Engl J Med NEJMoa2109072 (2021) doi:10.1056/NEJMoa2109072. ↩
- Antonelli, M. et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: a prospective, community-based, nested, case-control study. The Lancet Infectious Diseases S1473309921004606 (2021) doi:10.1016/S1473-3099(21)00460-6. ↩
- Hampshire, A. et al. Cognitive deficits in people who have recovered from COVID-19. EClinicalMedicine 101044 (2021) doi:10.1016/j.eclinm.2021.101044. ↩
- Del Brutto, O. H. et al. Cognitive decline among individuals with a history of mild symptomatic SARS‐CoV‐2 infection: A longitudinal prospective study nested to a population cohort. Eur J Neurol ene.14775 (2021) doi:10.1111/ene.14775. ↩
- (preprint) Douaud, G. et al. Brain imaging before and after COVID-19 in UK Biobank. http://medrxiv.org/lookup/doi/10.1101/2021.06.11.21258690 (2021) doi:10.1101/2021.06.11.21258690. The pre-print was later revised in August 2021. ↩
- Bonferonni corrected Family Wise Error (FWE). ↩
- The False Discovery Rate (FDR) correction. ↩
- G. A. Erausquin et al., “The chronic neuropsychiatric sequelae of COVID‐19: The need for a prospective study of viral impact on brain functioning,” Alzheimer’s & Dementia, vol. 17, no. 6, pp. 1056–1065, Jun. 2021, doi: 10.1002/alz.12255. ↩
- E. Guedj et al., “18F-FDG brain PET hypometabolism in post-SARS-CoV-2 infection: substrate for persistent/delayed disorders?,” Eur J Nucl Med Mol Imaging, vol. 48, no. 2, pp. 592–595, Feb. 2021, doi: 10.1007/s00259-020-04973-x. ↩
- Guedj, E. et al. 18F-FDG brain PET hypometabolism in patients with long COVID. Eur J Nucl Med Mol Imaging 48, 2823–2833 (2021). ↩
- Hosp, J. A. et al. Cognitive impairment and altered cerebral glucose metabolism in the subacute stage of COVID-19. Brain 144, 1263–1276 (2021). ↩
- Zhu, N. et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med 382, 727–733 (2020). ↩
- Scudellari. News Feature: How the coronavirus infects cells — and why Delta is so dangerous. Nature News. 28 July 2021. https://www.nature.com/articles/d41586-021-02039-y ↩
- Bar-On, Y. M., Flamholz, A., Phillips, R. & Milo, R. SARS-CoV-2 (COVID-19) by the numbers. eLife 9, e57309 (2020). ↩
- J. Hu, J. Jolkkonen, and C. Zhao, “Neurotropism of SARS-CoV-2 and its neuropathological alterations: Similarities with other coronaviruses,” Neuroscience & Biobehavioral Reviews, vol. 119, pp. 184–193, Dec. 2020, doi: 10.1016/j.neubiorev.2020.10.012. ↩
- C. McQuaid, M. Brady, and R. Deane, “SARS-CoV-2: is there neuroinvasion?,” Fluids Barriers CNS, vol. 18, no. 1, p. 32, Jul. 2021, doi: 10.1186/s12987-021-00267-y. ↩
- E. Chekol Abebe, T. Mengie Ayele, Z. Tilahun Muche, and T. Asmamaw Dejenie, “Neuropilin 1: A Novel Entry Factor for SARS-CoV-2 Infection and a Potential Therapeutic Target,” BTT, vol. Volume 15, pp. 143–152, May 2021, doi: 10.2147/BTT.S307352. ↩
- Xu, J. & Lazartigues, E. Expression of ACE2 in Human Neurons Supports the Neuro-Invasive Potential of COVID-19 Virus. Cell Mol Neurobiol (2020) doi:10.1007/s10571-020-00915-1. ↩
- Sender, R. et al. The total number and mass of SARS-CoV-2 virions. Proc Natl Acad Sci USA 118, e2024815118 (2021). ↩
- J. Buchrieser et al., “Syncytia formation by SARS‐CoV‐2‐infected cells,” EMBO J, vol. 39, no. 23, Dec. 2020, doi: 10.15252/embj.2020106267. ↩
- Z. Zhang et al., “SARS-CoV-2 spike protein dictates syncytium-mediated lymphocyte elimination,” Cell Death Differ, vol. 28, no. 9, pp. 2765–2777, Sep. 2021, doi: 10.1038/s41418-021-00782-3. ↩
- The following article provides an excellent overview of the infection process: https://www.nature.com/articles/d41586-021-02039-y ↩
- Artistic Animation of SARS-CoV-2 entry into human host-cell. https://www.youtube.com/watch?v=Xuc9D4LVJdg ↩
- P. E. Marik, J. Iglesias, J. Varon, and P. Kory, “A scoping review of the pathophysiology of COVID-19,” Int J Immunopathol Pharmacol, vol. 35, p. 205873842110480, Jan. 2021, doi: 10.1177/20587384211048026. ↩
- For further reading that isn't an academic paper, this April 2020 article from Science AAAS "A rampage through the body" by Wadman et al is older, but contains a fairly good description of the disease process and some impacted organs. This February 2021 article, "What it's like to die from COVID-19" by Katherine Harmon Courage describes the experience of severe disease. ↩
- N. J. Matheson and P. J. Lehner, “How does SARS-CoV-2 cause COVID-19?,” Science, vol. 369, no. 6503, pp. 510–511, Jul. 2020, doi: 10.1126/science.abc6156. ↩
- M. Gandhi and G. W. Rutherford, “Facial Masking for Covid-19 — Potential for ‘Variolation’ as We Await a Vaccine,” New England Journal of Medicine, vol. 383, no. 18, p. e101, Oct. 2020, doi: 10.1056/NEJMp2026913. ↩
- N. K. Sharma, S. Sarode, and G. Sarode, “Natural vaccines accumulated in face masks during COVID-19: Underappreciated role of facial masking,” Journal of Oral Biology and Craniofacial Research, vol. 12, no. 1, pp. 42–44, Jan. 2022, doi: 10.1016/j.jobcr.2021.10.001. ↩
- P. Kushalnagar, C. C. Chow, and A. Bax, “Self‐infection with speech aerosol may contribute to COVID‐19 severity,” J Intern Med, vol. 290, no. 6, pp. 1275–1277, Dec. 2021, doi: 10.1111/joim.13370. ↩
- H. A. Baker, S. A. Safavynia, and L. A. Evered, “The ‘third wave’: impending cognitive and functional decline in COVID-19 survivors,” British Journal of Anaesthesia, vol. 126, no. 1, pp. 44–47, Jan. 2021, doi: 10.1016/j.bja.2020.09.045. ↩
- J. Xu and E. Lazartigues, “Expression of ACE2 in Human Neurons Supports the Neuro-Invasive Potential of COVID-19 Virus,” Cell Mol Neurobiol, Jul. 2020, doi: 10.1007/s10571-020-00915-1. ↩
- These are grown from induced pluripotent stem cells (iPS) that are created by inducing an adult cell to regain its ability to differentiate into other kinds of cells, not from embryonic tissue. ↩
- E. Song et al., “Neuroinvasion of SARS-CoV-2 in human and mouse brain,” Journal of Experimental Medicine, vol. 218, no. 3, p. e20202135, Mar. 2021, doi: 10.1084/jem.20202135. ↩
- A. S. Zubair, L. S. McAlpine, T. Gardin, S. Farhadian, D. E. Kuruvilla, and S. Spudich, “Neuropathogenesis and Neurologic Manifestations of the Coronaviruses in the Age of Coronavirus Disease 2019: A Review,” JAMA Neurol, vol. 77, no. 8, p. 1018, Aug. 2020, doi: 10.1001/jamaneurol.2020.2065. ↩
- D. H. Brann et al., “Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia,” SCIENCE ADVANCES, p. 20, Jul. 2020, doi: 10.1126/sciadv.abc5801. ↩
- J. Xu et al., “The Role of the Gastrointestinal System in Neuroinvasion by SARS-CoV-2,” Front. Neurosci., vol. 15, p. 694446, Jul. 2021, doi: 10.3389/fnins.2021.694446. ↩
- T. Solomon, “Neurological infection with SARS-CoV-2 — the story so far,” Nat Rev Neurol, vol. 17, no. 2, pp. 65–66, Feb. 2021, doi: 10.1038/s41582-020-00453-w. ↩
- E. Uysal et al., “Chest CT findings in RT-PCR positive asymptomatic COVID-19 patients,” Clinical Imaging, vol. 77, pp. 37–42, Sep. 2021, doi: 10.1016/j.clinimag.2021.01.030. ↩
- P. Fine, K. Eames, and D. L. Heymann, “‘Herd Immunity’: A Rough Guide,” Clinical Infectious Diseases, vol. 52, no. 7, pp. 911–916, Apr. 2011, doi: 10.1093/cid/cir007. ↩
- W. Liu et al., “Predictors of Nonseroconversion after SARS-CoV-2 Infection,” Emerg. Infect. Dis., vol. 27, no. 9, pp. 2454–2458, Sep. 2021, doi: 10.3201/eid2709.211042. ↩
- (pre-print) B. A. Cohn, P. M. Cirillo, C. C. Murphy, N. Y. Krigbaum, and A. W. Wallace, “Breakthrough SARS-CoV-2 infections in 620,000 U.S. Veterans, February 1, 2021 to August 13, 2021,” Infectious Diseases (except HIV/AIDS), preprint, Oct. 2021. doi: 10.1101/2021.10.13.21264966. ↩
- Y. Bo et al., “Effectiveness of non-pharmaceutical interventions on COVID-19 transmission in 190 countries from 23 January to 13 April 2020,” International Journal of Infectious Diseases, vol. 102, pp. 247–253, Jan. 2021, doi: 10.1016/j.ijid.2020.10.066. ↩
- D. M. Hinton, “Emergency Use Authorization 091 (for REGEN-COV (casirivimab and imdevimab, administered together),” Sep. 09, 2021. Accessed: Oct. 24, 2021. [Online]. Available: https://www.regeneron.com/downloads/treatment-covid19-eua-fda-letter.pdf ↩
- M. Gruber, “EUA 27034/40 - Requests for Amendments to Update the Authorized Health Care Provider,” Jan. 06, 2021. Accessed: Dec. 01, 2021. [Online]. Available: https://www.fda.gov/media/144955/download ↩
- M. A. Malarkey and M. F. Gruber, “FDA Approval Letter for Comirnaty (Pfizer-BioNtech) COVID-19 mRNA Vaccine,” Aug. 23, 2021. [Online]. Available: https://www.fda.gov/media/151710/download ↩
- November 30, 2021: Antimicrobial Drugs Advisory Committee Meeting Announcement - 11/30/2021 - 11/30/2021 | FDA ↩
- Biden Administration announces U.S. government procurement of Merck’s investigational antiviral medicine for COVID-19 treatment (June 6, 2021) ↩
- Pfizer's Novel COVID-19 Oral Antiviral Treatment Candidate Reduced Risk of Hospitalization or Death by 89% in Interim Analysis of Phase 2/3 EPIC-HR Study (November 5, 2021) ↩
- S. S. Wolin, Democracy Incorporated: Managed Democracy and the Specter of Inverted Totalitarianism. Princeton University Press, 2008. ISBN 978-0-691-13566-3 ↩
- So rich that we can afford to treat vaccines like any other tossable consumer product with 15 million doses reported wasted out of 471 million administered (~3%, or about one in thirty-two). It’s not quite the picture of the depression-era farmer destroying crops while people starve, but I imagine people in countries without access to vaccines might see it that way. ↩